Introducing our Lived Experience As Expertise Series
Individuals with first-hand experience often have lots of ideas and solutions, but are not always positioned to share those on a path to impact. Philanthropy is uniquely positioned to acknowledge institutional oppression and to shift course, centering equity and countering oppression, enabling understanding and healing, while driving real solutions across the full spectrum of its work from strategy development to program operations, to monitoring, learning, and evaluation investments. Through this four-part series, you will see these mechanisms provide a crucial step to improving social outcomes. 
- Personal Interviews: With a guiding principle of “just listen,” we interviewed shelter residents to create programmatic solutions that vastly improved healthcare access for New Yorkers staying in the City’s shelter system.
- Focus Groups: In Los Angeles, focus groups engaged people with lived experience as partners, pushing our strategy forward to create meaningful social impact to improve the lives of vulnerable and marginalized communities.
- Lived Expertise Partnership: Prioritizing first-hand experience, we teamed with a professional with lived experience to address racial justice and criminal legal reform in New York.
- Inclusive Data Integration / Bayesian Analytics: Recognizing the importance of qualitative data and community knowledge to center equity and guide inclusive decision making, we engaged diverse voices to center racial equity in a research design framework.
Read on as we encourage you to consider how you guide your philanthropic approach.
Personal Interviews to Build Partnership: Checking Assumptions on Healthcare for the Unhoused
“People often tell us that we’re the authority and that we’re the expert and we know things. And we have to tell that part of our brain to shut up. And just listen.”
– Dan Treglia, PhD, researcher on homelessness
“Just listen” has been a guiding principle for our work with the Collaborative for Homeless Healthcare in New York. The lived experiences of people experiencing homelessness have too often been ignored by policymakers and practitioners, meaning that services intended to improve people’s lives frequently fail to meet their needs. Philanthropy’s failure to hear and understand the challenges facing homeless communities is especially noticeable in healthcare.
Roughly 60,000 people stay in New York City’s municipal homeless shelters on any given night. The single adults in the system tend to use the emergency department for medical care at over four times the rate of the non-homeless population. Typically, after calling 911, a homeless patient will endure long waits in the emergency room for care that they could have received more easily through other care providers. This wastes time for patients and providers, burdens people experiencing the many other stressors of homelessness, and denies patients the long-term care relationships that primary care and other providers could offer.
PERSONAL INTERVIEWS – Listening to find functional solutions
To address these challenges, the Collaborative for Homeless Healthcare decided to listen directly to homeless individuals to guide their strategy. With leaders in homeless healthcare, spanning doctors, public health experts, researchers, and City officials, the Collaborative is funded by The Leona M. and Harry B. Helmsley Charitable Trust and facilitated by Redstone. To meet the Collaborative’s mission to “improve the health and housing stability of homeless New Yorkers by ensuring they receive dignified, integrated, high-quality, person-centered care,” listening directly to clients is crucial.
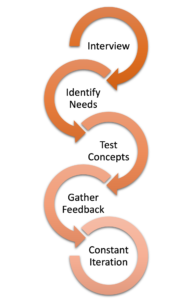
The group worked with Dan Treglia, PhD, a homelessness researcher at the University of Pennsylvania and a former staffer at the New York City Department of Homeless Services. In partnership with Redstone, Dan’s team interviewed 50 shelter residents about all aspects of their interactions with the healthcare system, from their relationships with care providers to the challenges of making appointments and finding transportation. The researchers listened attentively during the interviews and worked to earn the trust of their interviewees by meeting them in their shelters, developing relationships alongside trusted shelter staff, and making clear that the client’s personal experiences were of utmost concern to their research.
CHECK YOUR ASSUMPTIONS
Dan’s interview findings ran counter to several traditional assumptions about the healthcare preferences of those experiencing homelessness. Many shelter residents expressed interest in seeking primary care and an openness to using new technologies to access that care. Residents were also able to point to specific practical barriers – such as scheduling complications and lack of affordable and accessible transit – that kept them from accessing the care they knew they needed.
The Collaborative acted on this research by launching several pilots. One of them, the Nurse Triage Line, allows shelter residents and staff to speak with a live nurse 24/7 who can evaluate their symptoms and recommend the right care. Building off of what clients reported in interviews with Dan, the Nurse Triage Line offers on-demand telehealth appointments, which were previously assumed to be of limited interest to homeless clients, and free Uber Health rides to overcome the transit barrier for in-person appointments. In many cases, nurses connect clients to non-911 sources of care to address ailments without the stress, time, and other drawbacks of going to the emergency department.
Before the Nurse Triage Line was launched, Redstone held focus groups with shelter residents and staff to test the concept and figure out whether people would find the service useful. Feedback from those conversations informed the line’s key functions, ranging from the need for immediate nurse response to the ease of scheduling rides.
PERSONAL CONNECTION & RESPONSIVENESS
Checking assumptions directly with shelter residents has not stopped in the planning phase. Once the line was launched, a Project Coordinator was hired to spend time in the field with shelter residents and staff. This position serves an invaluable role to gather feedback and concerns from users, answer their questions, and identify ways to improve the service through constant iteration. With a Project Coordinator in place, we can anticipate and discover when something that seemed to make sense on paper is not going to work on the ground – whether a screening question residents cannot answer, a piece of equipment that shelters lack, or anything else.
This on-ground insight, the Collaborative’s flexible structure, and Redstone’s management expertise has allowed the team to rapidly adapt, identify, and test solutions to improve operations. On top of that, individual relationships with clients and staff help surface opportunities to get residents and staff excited about the new service – whether it’s branded pill boxes for residents or a tray of sandwiches for staff working the overnight shift.
CONTINUE TO GATHER FEEDBACK
The Collaborative’s work in New York City reminds us of the importance of hearing and internalizing the lived experiences of vulnerable populations when designing interventions. As we learned, partnerships are made stronger by dedicated trust-building in communities, a keen listening ear, and the willingness to check your assumptions at the door.
Watch for our upcoming Lived Experience As Expertise posts. Up next, we discuss how focus groups provided insider knowledge in Los Angeles. In August we will share how a professional with lived experience helped inform our strategy. And after that we will show how Bayesian analytics integrate and elevate data sourced from community knowledge to drive meaningful and robust solutions.